A compassionate guide to early detection, timely treatment, and lifelong vision protection.
What Is Glaucoma?
Glaucoma is a progressive eye disease that causes damage to the optic nerve, most often due to elevated intraocular pressure (IOP). It is one of the leading causes of irreversible vision loss worldwide. The optic nerve, which connects the eye to the brain, is composed of over a million delicate nerve fibers. When eye pressure builds up beyond normal levels, it can damage these fibers, initially affecting peripheral (side) vision and, over time, compromising central vision as well. This damage is permanent and cannot be reversed. However, with early diagnosis and appropriate treatment, further deterioration can often be slowed or halted.
Why Glaucoma Often Goes Undetected
Glaucoma is often called the “silent thief of sight” because it typically develops slowly and painlessly. Most patients experience no symptoms until significant vision loss has already occurred. By the time central vision is affected, the damage is usually advanced. For this reason, routine eye exams are essential, especially for individuals over the age of 40 or those with known risk factors.
Risk Factors You Should Be Aware Of
Several factors can increase the risk of developing glaucoma. Advancing age, especially beyond 40, is a key contributor. A family history of glaucoma, elevated intraocular pressure, and underlying systemic conditions like diabetes and hypertension can also elevate risk. Long-term steroid use, previous eye surgeries or trauma, and specific anatomical features such as thin corneas or narrow drainage angles further predispose individuals. Importantly, glaucoma can also affect those with no known risk factors or symptoms, making regular checkups all the more critical.
Types of Glaucoma
The most common form is Primary Open-Angle Glaucoma, where drainage channels gradually become less efficient, leading to a slow rise in eye pressure. Another form, Angle-Closure Glaucoma, occurs more suddenly when the drainage angle becomes blocked, causing a rapid spike in IOP. This can lead to acute symptoms such as severe eye pain, redness, blurred vision, nausea, or halos around lights—and requires immediate attention. Other types include Normal Tension Glaucoma, Secondary Glaucoma, and Congenital Glaucoma, each with its specific causes and characteristics.
How Glaucoma Is Diagnosed
At Dr. Pooja Khetarpal’s Eye Clinic, we employ a comprehensive set of tools to detect and monitor glaucoma. These include:
- Tonometry, to measure intraocular pressure
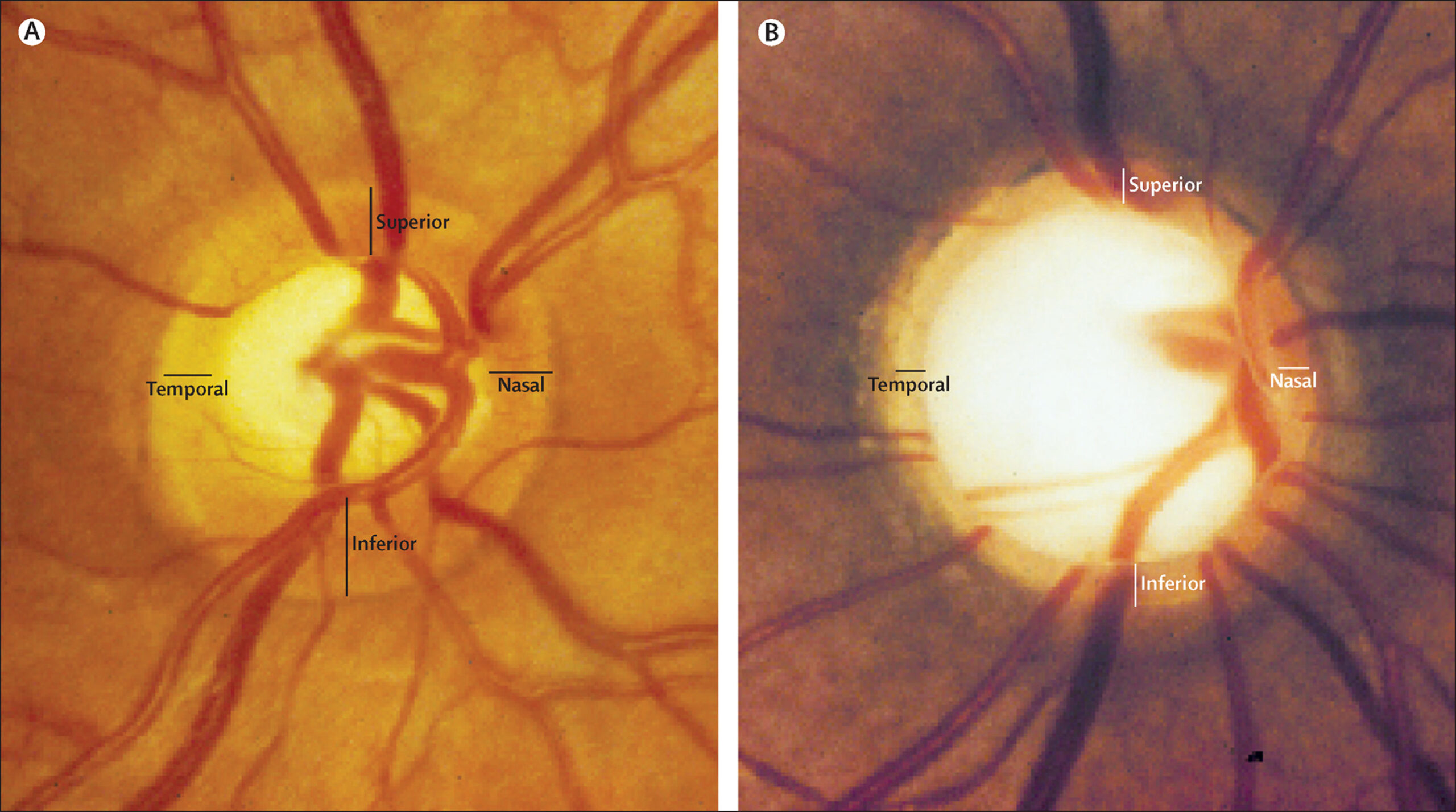
- Ophthalmoscopy, to examine the optic nerve for damage
- Visual field testing, to assess peripheral vision loss
- OCT (Optical Coherence Tomography), for detailed imaging of the optic nerve
- Gonioscopy, to evaluate the eye’s drainage angle
These tests are non-invasive and critical in both diagnosis and long-term monitoring.
Treatment Options for Glaucoma
While there is no cure for glaucoma, treatment focuses on lowering intraocular pressure to preserve remaining vision. The right approach depends on the type and stage of the disease.
1. Prescription Eye Drops
Often the first line of treatment, medicated drops help reduce IOP by either decreasing fluid production or improving its drainage. Common types include:
- Prostaglandin analogs (e.g., latanoprost): Increase fluid outflow
- Betablockers (e.g., timolol): Reduce fluid production
- Alpha agonists and carbonic anhydrase inhibitors, often used in combination
2. Oral Medications
When eye drops alone are insufficient, oral medications like acetazolamide (a carbonic anhydrase inhibitor) may be prescribed to further reduce eye pressure.
3. Laser Procedures
- Laser trabeculoplasty improves fluid drainage in open-angle glaucoma.
- Laser iridotomy creates a small hole in the iris to relieve pressure in cases of angle-closure glaucoma.
4. Surgical Treatment
- Trabeculectomy involves creating a new drainage pathway for fluid
- Glaucoma drainage implants help control pressure
- Minimally Invasive Glaucoma Surgery (MIGS) offers a quicker recovery with fewer complications for selected patients
Monitoring and Managing Glaucoma Over Time
Glaucoma requires lifelong management. Even after treatment, regular follow-ups are essential to track changes in vision and pressure. Routine assessments typically include pressure checks, optic nerve imaging, and visual field testing to detect subtle changes that may not be immediately noticeable. Consistency in taking prescribed medications and attending follow-up appointments is critical in preserving vision.
Frequently Asked Questions (FAQs)
What is normal eye pressure?
Normal intraocular pressure ranges from 10 to 21 mmHg. Pressures above this range may increase the risk of glaucoma, though damage can sometimes occur even within normal ranges.
Can optic nerve damage be reversed?
No. Damage to the optic nerve from glaucoma is permanent. However, further damage can be prevented or slowed with timely treatment.
Can you go blind from glaucoma?
Yes. If left untreated, glaucoma can lead to total vision loss. Early diagnosis and continued care are essential to prevent this outcome.
Is high eye pressure always a sign of glaucoma?
Not always. Some people have elevated pressure without nerve damage, a condition known as ocular hypertension. However, they remain at higher risk and must be monitored closely.
Final Word: Don’t Wait for Symptoms
Glaucoma can rob you of your vision quietly and permanently. That’s why early screening, proactive treatment, and lifelong monitoring are essential. If you’ve noticed any changes in peripheral vision, are above the age of 40, or have a family history of glaucoma, now is the time to act.
If you have experienced eye pain, vision disturbances, or sudden visual loss, especially symptoms associated with angle-closure glaucoma—don’t delay. Prompt diagnosis can prevent lasting damage.
At Dr. Pooja Khetarpal’s Eye Clinic, we combine precision diagnostics, evidence-based treatments, and compassionate care to help you protect what matters most, your vision.
Schedule your consultation with Dr. Pooja Khetarpal today
Contact us at Khetarpal Hospital today. Let’s take the first step toward preserving your sight together.